Your Microbiome – friend or foe?
Your Microbiome – friend or foe?
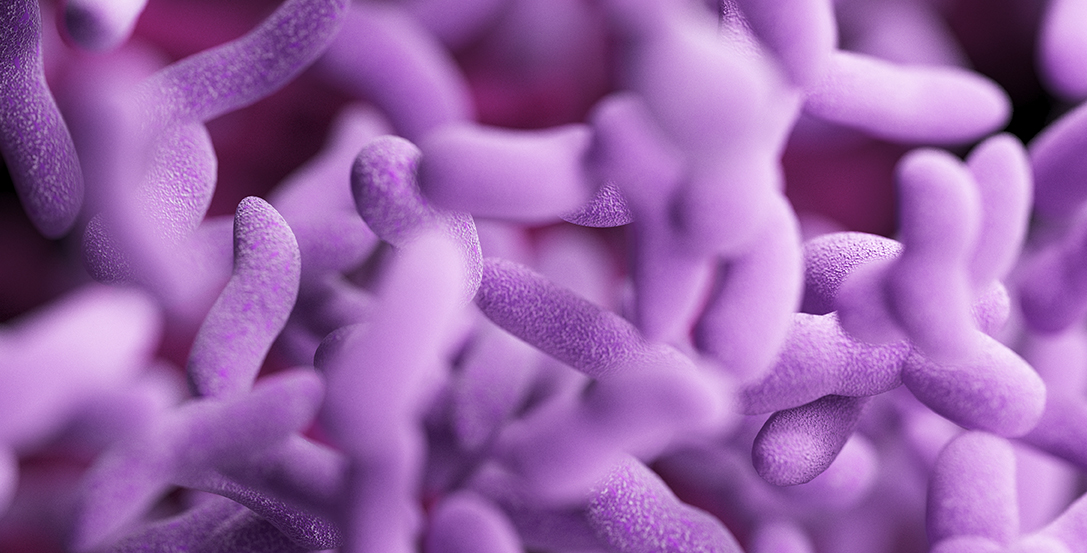
You may have heard the word ‘microbiome’ itself – denoting a whole range of organisms living in a given space in the body, from viruses, bacteria and fungi to bacteriophages or mutated viruses with bacteria which can also live happily next to specific single strains of organisms. You may have even tried some drinks and foods like kombucha, kefir or sauerkraut which have recently gained popularity as perfect gut microbiome boosting tools.
But do you know that your microbiome does not only exist in your gut? Yes, the gastric one has been in the headlines but every single one of us also has many others like respiratory, urinary, vaginal (if you are a woman), oral, skin, and ocular (in the eyes). In every area of the body lined by mucous membranes there is a specific gamete of organisms which reside there, and also – specific pathogenic (i.e. ill health inducing) organisms which gravitate to this area. For instance: parasites like Blastocystis tend to prefer the gut areas, whilst E.coli tends to prefer urinary tract – generally speaking.
Think of microbiome as your internal eco-environment: it can get damaged when exposed to adverse circumstances. And it does not need a single, large cataclysmic event to alter the balance within it – often the resulting damage to the delicate balance within it is a cumulative effect of small, specific factors. Starting as early as from conception, through the birthing process, early childhood, adulthood and later life. These range from:
During the first three years of life:
- maternal obesity, stress, and infections
- mode of delivery (vaginal vs. C-section), antibiotics used during labour
- feeding post-partum (breast milk vs formula)
- the gut-brain axis of the child / emotional traumas – birth related and since
- vaccination / any foreign substance that activates a baby’s immune system
Later in a child’s life:
- any stressful events
- antibiotic use
- weaning / use of processed foods since expanding the diet
- pesticides, herbicides, and other food additives
- any food poisoning / exposure to pathogens
- specific foods and bioactive food components (gluten & other lectins, grains, salicylates, glutamate, histamine, oxalates, FODMAPs, etc.)
Teens and adult life:
- antibiotic use, oral or even topical
- other medications including over-the counter ones (e.g. anti-acid meds, pain-killers, anti-depressants, etc.)
- hormonal preparations (e.g. acne creams, HRT and the pill)
- sugar and alcohol overuse / any recreational drugs
- eating junk food
- inorganic, highly chemicalised, intensively reared food produce
- nutritional deficiencies (e.g. nutrients needed for the integrity of the mucosal barrier)
Broadly speaking, the potentially ‘irritating’ compounds in foods as well as undigested food particles affect the integrity of the mucous membranes of the gut, leading to impaired immune responses, disturbed digestion and absorption (leaky gut), tendency to inflammation and propensity to reactions to foods otherwise expected to be tolerated by our digestive system. They also alter the prevalence of the desirable bacteria leading to dysbiosis (disturbed balance within the strain present in the gut) and compounding the aforementioned problems. Glutamate, for instance, can trigger an overgrowth of the undesirable strains
When a highly processed diet is consumed, it can lead to a permanent loss of bacteria critical for the proper functioning of the microbiome and increased levels of producing bacteria producing endotoxin and virulence factors. Scientists studying the gut microbiome have discovered unique microbial differences in patients with food allergies compared to the healthy group and postulated the dysbiosis of the microbiome to precede the development of food intolerance. Likewise, diets low in carbohydrates (e.g. various types of ketogenic approaches), have been shown to be usually low in fibre which is needed by the gut bacteria to make short chain fatty acids (SCFAs) which protect the gut lining, and thus the microbiome, help in its repair and are anti-inflammatory. However, in other cases, the ketogenic diet has been found to improve the diversity of the microbiome so the jury is still out on this one.
The last observation implies that our mucous membranes exhibit a biochemically specific approach to how our own environment interacts with the gut inhabitants within us, and that we still have a lot to learn about this interface. For the time being, we may all need to follow therapeutic, microbiome supporting diets that suit us individually. Such diets need to be tailored to our individual, specific requirements based on our unique biochemistry, health history, nutrient deficiencies, current condition of the microbiome, and – last but not least – genetics. Not only do they alleviate the distressing symptoms, they also help eliminate the triggers, repair the digestive and immune systems as well as rebuild microbiome naturally. Since imbalanced microbiomes have been found to be contributing to the development of several 21st century endemic health problems (from colon diseases and cancer, through cardio-vascular problems, dementias, chronic infections, to stress and ageing)
This is exactly where Body Mind Insights can be of assistance.

